Acid Reflux
Reflux and Causes

Reflux is really common.
Around 20% of us have regular symptoms.
Retrosternal (behind the breastbone), burning discomfort, rising up from the abdomen and heading towards your throat is the most common complaint. We call this heartburn.
Some people bring up food or fluid into their mouth, this is called acid or water brash and is caused by regurgitation. Others can feel food getting stuck due to the inflammation or causing pain on the way down. Rarely, some people get atypical reflux symptoms such as a chronic cough.
Essentially reflux is caused by the acid in your stomach ‘refluxing’ back into your oesophagus (food pipe). So some acid reflux is normal but too much or too often or the lining of the oesophagus, which is not acid resistant like the stomach lining, gets damaged.
We call this Gastro-Oesophageal Reflux Disease or GORD (in America it’s GERD, they can’t spell).
Hiatus Hernia

The commonest cause of reflux is a hiatus hernia.
This when the ‘hiatus’, the hole through the diaphragm (which is the big muscle between your chest and abdomen) that the oesophagus passes through into the abdomen is wider than it should be. This allows a bit of your stomach to slip into your chest and means that the lower oesophageal sphincter, that prevents reflux, can’t work properly. Hence acid can flow back into your oesophagus and cause reflux symptoms and damage your oesophagus.
A hiatus hernia may occur without reflux and reflux may occur without a hiatus hernia but they usually co-exist to an extent and when surgery is required they are treated together. We see reflux endoscopically as burns (oesophagitis). When scar tissue forms to repair your oesophagus this can tighten it, causing a ‘stricture’, or lead to your body trying to protect the oesophagus from the acid and change the lining to one like the stomach lining. We call this change Barrett’s oesophagus (named after an Aussie surgeon who worked in London, Sir Norman Barrett).
Once something in the body changes there is always a risk it can change again and become cancerous. Although that risk is really small, we consider Barrett’s Oesophagus to be a pre-malignant condition and recommend keeping a close eye on it if you have it.
Test and Investigations

If you get heartburn then you may be already using over the counter antacids such as Rennie’s or Gaviscon or your doctor may give you some stronger medication. If these don’t work or you have troublesome symptoms then you may need some investigations to see why.
We consider some symptoms as more worrying – this is if you are losing weight unintentionally, have persistent symptoms despite treatment, have trouble swallowing or food sticking, are anaemic, have closer relatives who have had oesophageal or gastric cancer or are over 55 years old. If this is the case then you warrant more urgent investigation.
I would nearly always recommend an endoscopy (or gastroscopy) first. This allows me to see if there are any burns to the oesophagus, any Barrett’s changes and assess if there is a hiatus hernia or other underlying problem. It also reassuringly helps to rule out cancers of the oesophagus and stomach which although uncommon are very serious.
Sometimes I ask for a radiology swallow test – this is often called a barium swallow but the radiologists may use a number of non-barium radiological dyes to do the test. This can give us different information as it is ‘dynamic’. So we can see a little how your oesophagus is working as well as assess for a hiatus hernia for example.
Finally, we may need to get some oesophageal physiology tests. These are much more sensitive tests of the function of the oesophagus – how it squeezes, how hard it squeezes and when, and also just how much acid is refluxing and when. We don’t have all these tests available in Jersey so this may require a trip to Southampton or Portsmouth.
Treatment for Reflux
If you go to your doctor with heartburn then they again will make sure that you have no worrying symptoms, we call these ‘alarm symptoms’ - to help rule out the rare cases where these symptoms are caused by an underlying cancer:
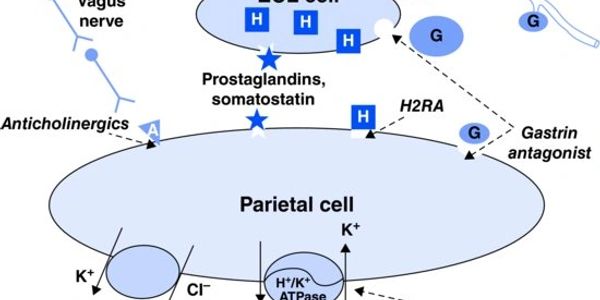
Otherwise, your doctor may suggest lifestyle changes such as stopping smoking, eating healthier foods and avoiding ones that cause your symptoms, not eating late at night and trying to lose some weight. Then they will start some amazing medication that has revolutionised acid problems: these are called the proton pump inhibitors or PPIs. There are 5 of these: omeprazole, pantoprazole, lansoprazole, rabeprazole and esomeprazole. They all use the same active component, imidazole, but have a different carrying molecules which affects the drugs and you in different ways. So they all work to reduce your stomach acid but one may work a little better than another or have different side-effects. I strongly advise taking these tablets 30 minutes away from anything else – food or other medication.
Perhaps take it as soon as you get up in the morning and leave breakfast for half an hour. There are an older class of drugs called H2-receptor antagonists but these are not as strong.
You can also continue to take antacids, like Gaviscon, in between doses (but again don’t do this for at least 30 minutes after taking your PPI).
PPIs have been around since the early 1990s and if your symptoms are controlled by PPIs then these are safe to take long-term but they do have some side-effects. They can change your gut flora and alter your absorption of certain vitamins and minerals particularly iron and calcium.
Anti-reflux Surgery

Cause not Effect
Anti-reflux surgery treats the cause (i.e. repairs your hiatus hernia so that you don’t reflux at all) rather than PPIs which treat the effect (i.e. you still reflux but with reduced acid in the fluid so you get less symptoms).
You may not want to take PPIs for life and can’t skip a dose or you get your symptoms back; or have side-effects or your symptoms persist despite the tablets.If this is the case then I need to make sure that your symptoms are genuinely due to acid reflux. So you will need an endoscopy, swallow test and maybe also oesophageal physiology testing before surgery.
There are a number of different operations for acid reflux. The best known is the group of surgeries called fundoplications. These developed from an operation called the Nissen fundoplication (after a brilliant surgeon called Rudolph Nissen who also operated on Albert Einstein – it’s a great story). The operation involves two steps: the first is a repair of the muscle of the hiatus using stitches. The second step wraps the top part of the stomach (fundus) around the lower part of the oesophagus. The classic Nissen version is a full 360 degree wrap but I frequently perform partial (180-270 degree wraps). This tightens up this valve area and stops reflux but also reduces the ability to belch or vomit. This can cause bloating after eating (gas bloat) and increased wind (flatus). This is the reason for the partial wraps, they cause less side effects.
There are lots of different ways of doing these so I’m happy to discuss them all and choose the best balance of operation for you and your symptoms. I’ve just spent the last 8 years in the centre where many of these operations were devised!

Anti-Reflux Treatments. How?
All of these are performed laparoscopically (by keyhole) with 5 little cuts on your abdomen under GA. They usually take about an hour to perform, with one night in hospital.
Basically, I repair your hiatus hernia if you have one then wrap the top part of the stomach around your lower oesophagus to form a physiological barrier to acid reflux.
There are some surgical alternatives to a fundoplication – there is a new operation using a magnetic ‘necklace’ that is wrapped around the lower oesophagus (LINX procedure) and if you have weight issues then we can consider a Roux-en-Y Gastric Bypass, which is arguably the best operation for reflux that we have as all the acidic juices from the stomach are diverted away from your oesophagus.
We can discuss these options.
However, fundoplications are quite simply one of the most effective operations that we can do. It’s quick, it’s easy to recover from, it’s safe and it’s reversible. The satisfaction ratings for the procedure are consistently between 90-95%. By far the majority of patients are ‘cured’ of their reflux long-term. But there is always some drift, so some patients (around 20%) do have reflux symptoms return and ultimately go back on to PPIs, albeit at a lower dose and with better reflux control.
But despite the success, like all treatments, these operations do come with side-effects: the most classical is dysphagia (trouble with food sticking). There is a technical balance point with this surgery – the fundoplication has to be tight enough to stop reflux but not too tight or it will cause food to stick. Nearly everyone has some feeling of tightness for the first six weeks or so and should stay on soft or sloppy foods.
As a result, most patients lose 5-10kg of weight with the change in diet. Gradually, as swelling reduces, you can eat more normally but most people will still avoid really solid foods like lumps of steak.

Anti-Reflux Surgery. Risks?
If you get troublesome swallowing difficulties then this can be cured by an endoscopic stretch of the repair site and rarely revisional surgery. Many patients get gas bloat after eating as it can be difficult to belch and release the gas that you swallow naturally with every mouthful. This can also mean that you pass more flatus. That sounds amusing, but it can be socially damaging for some people. Overall re-operation for post-operative issues or recurrent reflux in the longer term runs at around 5-10%.
It’s a very safe surgery, nearly always manageable laparoscopically, even complex revisional surgery is done this way, but there are risks with any operation such as bleeding, infection, scarring and conversion to an open operation. The spleen also lies very close to the stomach and in theory can be damaged by the surgery and have to be removed. I’ve never personally had this happen but I have seen it happen when an extremely experienced surgeon was operating. So never say never.
Complications and side-effects
- Recurrent hiatus hernia or slippage of the wrap (uncommon)
- Injury to lung and pneumothorax (uncommon)
- Wound infection (uncommon)
- Bleeding (uncommon)
- Need for splenectomy (rare)
- Perforation and peritonitis (uncommon)
- Deep vein thrombosis and pulmonary embolism (uncommon)
- Heart attack (uncommon)
- Chest infections (uncommon)
- Death (rare)
- Delayed stomach emptying - gastroparesis (uncommon)
- Persistent food sticking sensation (common)
- Late recurrent reflux symptoms (uncommon)
Video
Check out this great video
finesurgery | YOUR Clinic in Jersey
Suite 3.2, lido medical centre, st saviour, Jersey, je2 7la